Despite examining test data from over 10,000 patients nationwide, researchers were unable to identify any distinctions between individuals with and without long-term COVID-19.
Researchers found that Long Covid is still difficult to diagnose, according to a study that was released on Monday in the Annals of Internal Medicine.
The results are a part of the RECOVER Initiative of the National Institute of Health, a multibillion dollar project that was started in 2021 to uncover causes and solutions for the estimated 17 million Americans who have long-term COVID-19.
Data from almost 10,000 patients at 83 clinical locations throughout the nation were included in Monday’s research. The patients’ usual blood counts, the outcomes of their kidney and liver tests, and indicators of inflammation in the body were among the many lab data that the researchers examined. Between individuals with long-term COVID-19 and those without the illness, they did not find any changes.
Lead research author Dr. Kristine Erlandson, an infectious disease specialist at the University of Colorado Anschutz Medical Campus, expressed disappointment that a test to identify long-term Covid could not be developed.
Erlandson stated, “I believe it is consistent with what we have learned more recently.” “It’s really a symptom-driven condition, and diagnosing someone with long-term COVID is based on specific laboratory values rather than a specific definition.”
Physicians at the Johns Hopkins University School of Medicine stated in an accompanying editorial that “clinicians are left to continue doing what we have done in the past: order tests to rule out alternative explanations rather than to diagnose long COVID.”
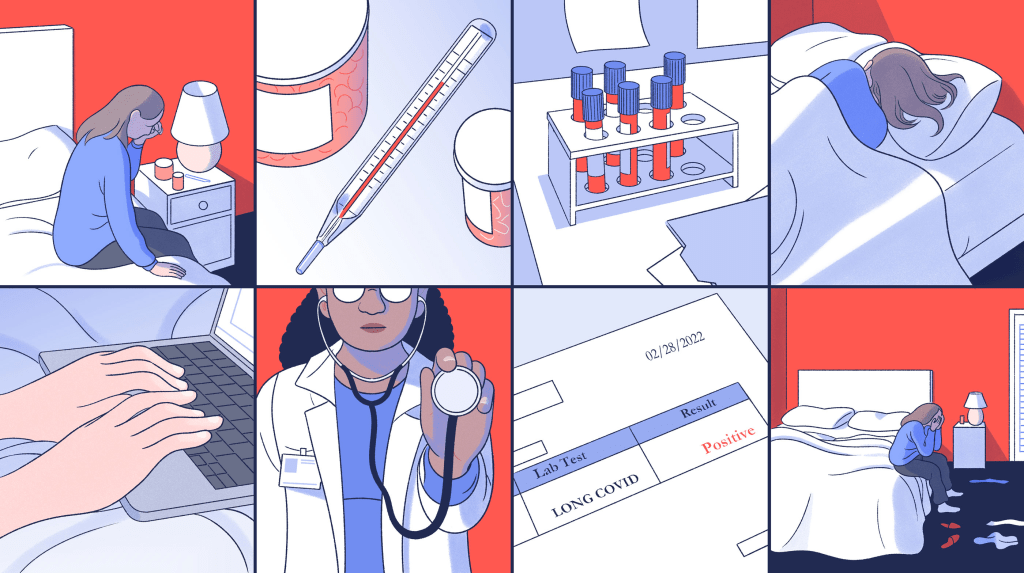
Based on a grading system of 12 symptoms, including palpitations, brain fog, and dizziness, among others, patients in the research were classified as having long-term COVID-19. Various symptoms were assigned varying ratings, and if the score reached a threshold of 12, a lengthy Covid diagnosis was satisfied.
A positive Covid test result was not necessary for diagnosis, nor was there a time limit for symptoms.
Pulmonologist Dr. Marc Sala, co-director of Northwestern Medicine’s Comprehensive Covid Center, praised the study’s quality but pointed out that the findings may disappoint the millions of people who are still afflicted.
“One possible critique of the study, in my opinion, is that many of the lab tests they sent are identical to what you would receive from your primary care physician,” Sala stated. “Many of these tests weren’t very sophisticated in their search for a new explanation for prolonged Covid.”
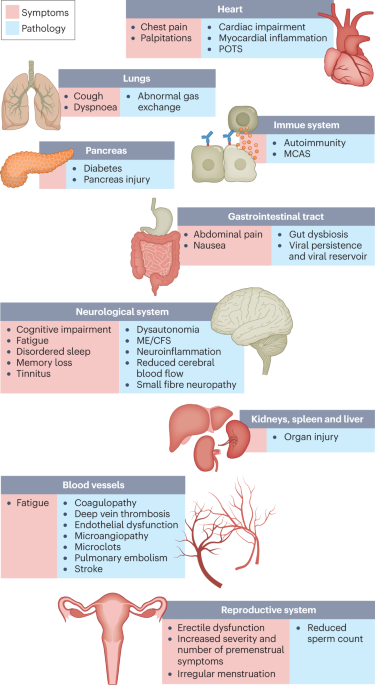
While regular blood tests are frequently normal in Sala’s long-term Covid patients, more specialized testing, like as blood tests conducted during physical activity or a CT scan following Covid pneumonia, might reveal abnormalities. According to him, patients would require far more testing than what was done in the research, especially if they are generally healthy and present with very high levels of exhaustion and dyspnea.
The study’s author, Erlandson, stated that further specialized testing is being carried out as part of ongoing research for the RECOVER Initiative, and that this research is only the beginning.
Having worked with long Covid patients for three years, Dr. Nisha Viswanathan, the head of UCLA Health’s long Covid clinic, was not shocked by the outcomes.

“One of the most startling aspects of long-term COVID is that, despite negative results from at least our standard medical examinations, our patients are still experiencing symptoms,” stated Viswanathan.
She expressed hope that a biomarker for long-term COVID-19 illness would eventually be discovered and cited a recent preprint—a non-peer-reviewed study—from Yale School of Medicine that shown elevated levels of autoantibodies—antibodies that target the body rather than foreign objects—as a possible indicator.